What Is Osteochondritis Dissecans?
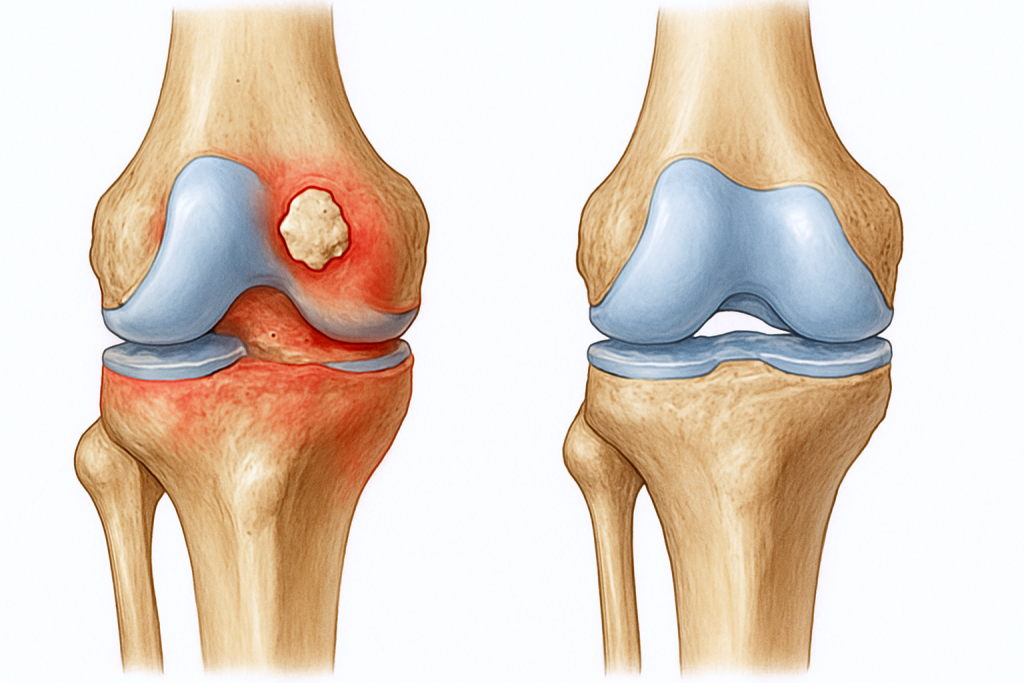
Osteochondritis Dissecans (OCD) is a joint condition in which a fragment of bone beneath the cartilage loses its blood supply, causing both the bone and the overlying cartilage to potentially loosen and separate from the surrounding tissue. This condition most commonly affects the knee—particularly the femoral condyles—but can also impact other joints such as the elbow or ankle.
OCD often affects adolescents and young adults, especially athletes. If left untreated, the condition may progress to cartilage breakdown, joint instability, or early-onset osteoarthritis.
What Causes OCD?
The exact cause of OCD is not fully understood, but it is believed to result from repetitive microtrauma—minor but repeated injuries that interfere with normal blood flow to the bone beneath the cartilage. Other contributing factors may include:
-
High-impact or repetitive sports activities
-
Genetic predisposition
-
Growth-related stress during adolescence
-
Joint malalignment or instability
-
Prior trauma or injury
In young patients whose bones are still developing (skeletally immature), OCD lesions may heal on their own. In older teens and adults, healing without intervention is less likely.
Common Symptoms of OCD
Patients with osteochondritis dissecans of the knee may experience:
-
Vague, aching knee pain during or after activity
-
Swelling and tenderness over the joint
-
Stiffness or reduced range of motion
-
Clicking or popping sounds
-
Locking or catching sensation (if a loose fragment is present)
-
Feeling of joint instability or “giving out”
Symptoms tend to worsen with prolonged activity or weight-bearing and often improve with rest.
How OCD Is Diagnosed
At Kerlan Jobe Institute, we use a combination of clinical evaluation and advanced imaging to diagnose OCD:
-
Physical Examination: We assess joint tenderness, range of motion, mechanical symptoms, and swelling.
-
X-rays: Help detect the presence of a lesion and evaluate the stage of development or fragmentation.
-
MRI: Essential for visualizing the stability of the lesion, cartilage integrity, and bone marrow changes.
-
CT scan (in select cases): May be used to assess bone fragment position and healing potential in surgical planning.
OCD Grading & Lesion Stability
OCD is categorized by stability (whether the cartilage and bone fragment are still attached) and skeletal maturity (whether growth plates are still open). These factors help determine the best treatment plan.
-
Stable lesions in growing individuals may resolve with rest and activity modification.
-
Unstable lesions or those in adults often require surgical intervention.
Treatment Options
Non-Surgical Treatment (for Stable Lesions in Youth)
-
Activity modification (avoid impact sports)
-
Bracing or crutches to offload weight from the knee
-
Physical therapy to maintain range of motion and strength
-
Periodic imaging to monitor healing over 3–6 months
Many adolescents with stable OCD lesions show full recovery with conservative care if diagnosed early.
Surgical Treatment (for Unstable or Symptomatic Lesions)
Surgery is considered when:
-
The lesion is unstable or detached
-
Symptoms persist despite non-operative care
-
The patient is skeletally mature (growth plates are closed)
Surgical options offered at Kerlan Jobe Institute include:
-
Arthroscopic drilling: Stimulates healing by increasing blood flow to the lesion.
-
Internal fixation: Reattaches a loose bone and cartilage fragment using bioabsorbable pins or screws.
-
Cartilage repair or replacement:
-
Microfracture or osteochondral autograft transplantation (OAT) for small, contained lesions.
-
Autologous chondrocyte implantation (ACI) for larger or irregular defects.
-
-
Osteotomy: Realigns the knee to reduce stress on the damaged area, in select cases with malalignment.
Recovery and Outlook
Recovery timelines depend on the treatment type and lesion severity:
-
Non-surgical patients: May return to sports within 3–6 months if healing is confirmed.
-
Surgical patients: Typically require 4–9 months of rehab, including restricted weight-bearing, physical therapy, and imaging follow-up.
Early diagnosis and treatment of OCD can lead to full recovery in many cases. At Kerlan Jobe Institute, our orthopedic specialists use the latest surgical and regenerative techniques to preserve the knee joint and support long-term function.