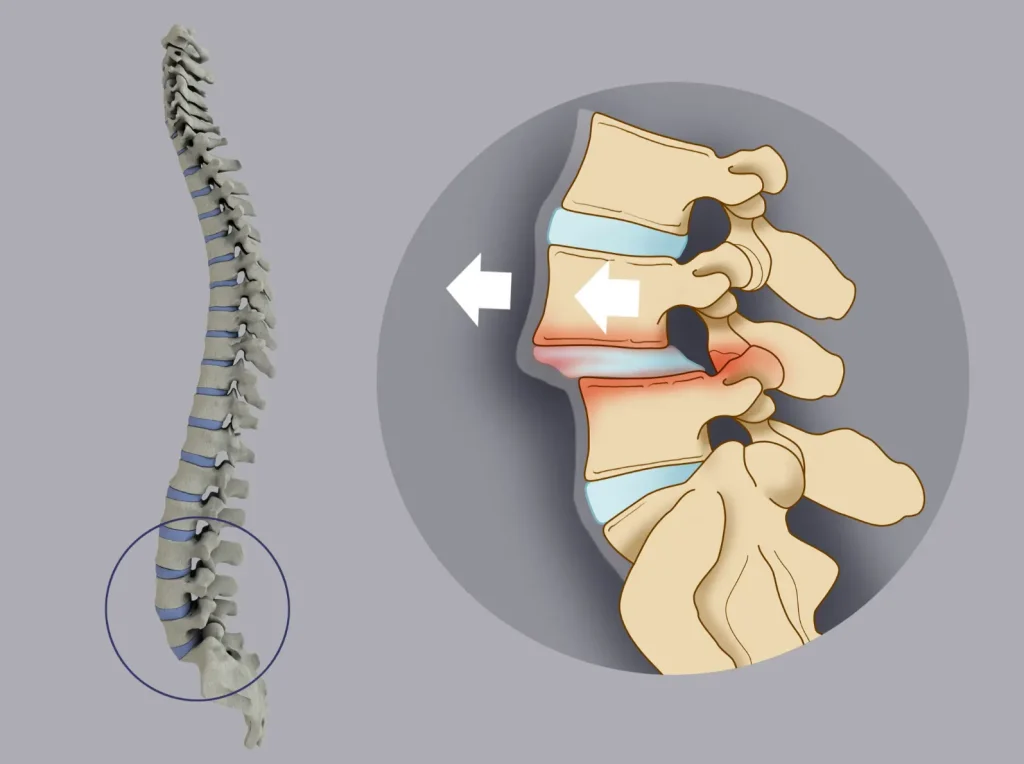
Unstable Motion Between Vertebrae Leading to Lower Back Pain and Dysfunction
What Is Lumbar Instability?
Lumbar instability refers to excessive or abnormal movement between vertebrae in the lower spine. This condition can result from injury, degeneration, or congenital issues and often leads to mechanical back pain, nerve irritation, or functional limitations. Unlike static deformities, instability typically presents with symptoms that fluctuate depending on posture and activity level.
Causes and Risk Factors
- Age-related degeneration of spinal discs and joints
- Prior spinal surgery (post-laminectomy instability)
- Trauma or vertebral fractures
- Spondylolysis or spondylolisthesis
- Congenital or connective tissue disorders (e.g., Ehlers-Danlos Syndrome)
- Repetitive strain or poor core muscle support
Symptoms
- Recurrent or chronic lower back pain that worsens with movement or prolonged positions
- “Catching” or sharp pain with certain motions like bending or twisting
- Sensation of spinal shifting or giving way
- Muscle fatigue or spasms in the lower back
- Occasionally, nerve-related leg symptoms if instability irritates spinal nerves
Diagnosis
- Clinical evaluation of spinal motion, alignment, and neurologic function
- Imaging studies:
- Flexion-extension X-rays to detect abnormal vertebral motion
- MRI to assess soft tissues, discs, and nerve involvement
- CT scan may help in evaluating subtle bony abnormalities
Treatment
Non-Surgical Treatment
- Often the first approach for mild to moderate instability
- May include:
- Physical therapy to strengthen core and paraspinal muscles
- Avoidance of provocative movements or activities
- Bracing to limit excessive spinal motion in acute phases
- NSAIDs or muscle relaxants for symptom relief
Surgical Treatment
- Recommended when instability causes significant pain or nerve symptoms unresponsive to conservative care
- Surgical options may involve:
- Spinal fusion to stabilize the affected segments
- Instrumentation (rods, screws) to support fusion
- Decompression procedures if nerve roots are compressed
Recovery Timeline
- Non-surgical improvement may take 6–12 weeks with structured rehabilitation
- After spinal fusion:
- Initial recovery: 4–6 weeks of reduced activity and bracing
- Gradual return to function over 3–6 months
- Full spinal fusion may take up to 12 months for complete healing and stabilization
Expert Treatment at Kerlan Jobe Institute
The spine care team at Kerlan Jobe Institute is experienced in evaluating and managing lumbar instability. From advanced diagnostics to minimally invasive surgical solutions, we tailor treatment to help patients regain spinal stability, reduce pain, and improve mobility.