Lower Back Pain from a Bulging or Ruptured Spinal Disc
What Is a Lumbar Herniated Disc?
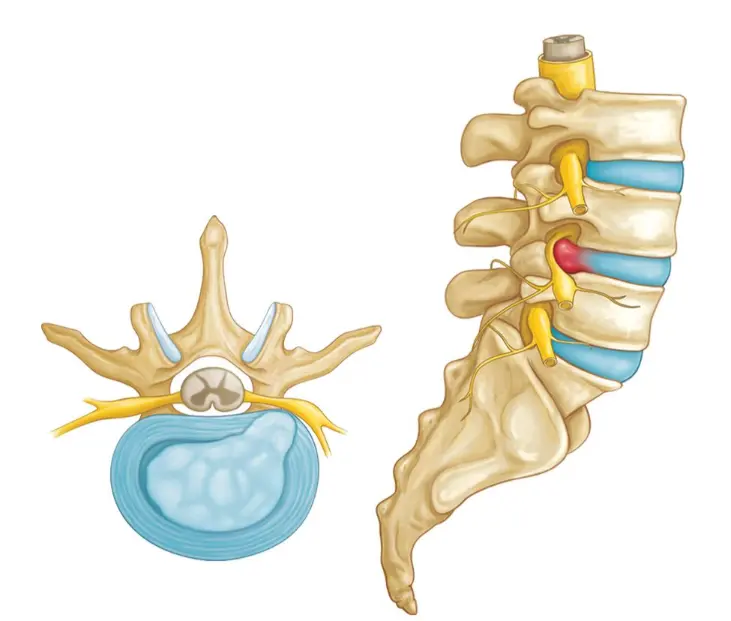
A lumbar herniated disc occurs when the soft inner gel of a spinal disc (nucleus pulposus) pushes through a tear or weakness in its tough outer layer (annulus fibrosus), typically in the lower back. This protrusion can compress nearby spinal nerves, resulting in pain, numbness, or weakness that radiates down the leg — a condition commonly known as sciatica.
Herniated discs are most frequently found between the L4–L5 or L5–S1 vertebrae and are a common cause of lower back and leg pain in adults.
Causes and Risk Factors
- Age-related disc degeneration (natural wear and tear)
- Sudden lifting, twisting, or bending motions
- Repetitive heavy lifting or poor lifting mechanics
- Prolonged sitting or sedentary lifestyle
- Obesity (increased stress on spinal discs)
- Smoking (reduces disc nutrition and healing capacity)
- Genetic predisposition to disc problems
Symptoms
Symptoms vary depending on the location and severity of the herniation and which nerve roots are affected:
- Lower back pain (may be constant or intermittent)
- Radiating pain down one leg (sciatica)
- Numbness or tingling in the buttock, thigh, calf, or foot
- Muscle weakness in the leg or foot
- Difficulty standing, walking, or performing daily activities
- Increased symptoms with sitting, coughing, or sneezing
Diagnosis
- Physical exam: Neurologic testing of strength, reflexes, and sensation
- Straight leg raise test (may reproduce radiating pain)
- MRI: The gold standard for visualizing disc herniation and nerve compression
- CT scan: Useful in patients who cannot undergo MRI
- Electromyography (EMG): May be used to assess nerve involvement if diagnosis is unclear
Treatment
Non-Surgical Treatment
- Activity modification and short-term rest
- Nonsteroidal anti-inflammatory drugs (NSAIDs) or oral steroids
- Physical therapy: Stretching, core strengthening, and posture correction
- Epidural steroid injections: May reduce inflammation and nerve irritation
- Most patients improve within 6–12 weeks without surgery
Surgical Treatment
- Reserved for patients with severe or persistent symptoms, progressive neurological deficits, or failure of conservative treatment
- Microdiscectomy: Minimally invasive removal of the herniated disc material pressing on the nerve
- Laminectomy (in select cases): Removal of a small portion of bone to relieve pressure
- Surgery aims to reduce pain, restore function, and prevent long-term nerve damage
Recovery Timeline
- Non-surgical patients typically improve within a few weeks to 3 months
- Post-surgical recovery may involve:
- Light activity within 1–2 weeks
- Physical therapy beginning around 4–6 weeks
- Return to work (non-physical): ~2–4 weeks post-op
- Full return to physical labor or sports: 8–12 weeks depending on recovery
Expert Treatment at Kerlan Jobe Institute
At Kerlan Jobe Institute, our spine specialists are experienced in diagnosing and treating lumbar herniated discs with both conservative and surgical approaches. Whether you’re an athlete or a working professional, we create a personalized care plan focused on relieving pain, restoring movement, and getting you back to an active lifestyle safely.